Journal of Medical Sciences and Health Care Research

Case Report - (2022) Volume 1, Issue 1
Congenital Diaphragmatic Hernia in Childhood - A Case Report
Received Date: Nov 28, 2021 / Accepted Date: Jan 10, 2022 / Published Date: Jan 17, 2022
Abstract
Introduction: Congenital diaphragmatic hernia is multi factorial congenital defect in diaphragm, though rare it is a differential diagnosis for neonatal distress. It is not reported in childhood.
Case presentation: Here I am going to present 6 year old male child presented with cough and going stress as congenital diaphragmatic hernia is going to be a differential diagnosis for childhood chest problems as well.
Conclusion: It is good to consider congenital diaphragmatic hernia in children presented with repeated chest infection like complaints.
Keywords
Congenital, Diaphragmatic hernia, Chest infection, Pneumonia, Tuberculosis, Chest x-ray
Abbreviations: CDH: Congenital Diaphragmatic Hernia; CAP: Community Acquired Pneumonia; TASH: Tikuranbessa Specialized Hospital; DS: Down Syndrome; SNHL: Sensori Neural Hearing Loss
Introduction
The earliest English language description of the gross anatomy and pathophysiology associated with Congenital Diaphragmatic Hernia (CDH) in a newborn was by McCauley, an associate of Hunter, as reported in the Proceedings of the Royal College of Physicians, 1754. Management and pathophysiology of congenital diaphragmatic hernia was not well known until 1940. Though bochdalk speculated the pathophysiology wrongly the commonest type of CDH is remained having its name [1].
In other researches, CDH was first described by Vincent Bochdalek from Chek in 1848, but first successful repair of CDH in a neonate was conducted by Gross in 1946 [2].
Congenital Diaphragmatic Hernia (CDH) is a complex developmental defect having a multifactorial etiology; in majority of cases (~80%), the cause is not known. Survival rates for patients with CDH have increased over the past decade with early prenatal detection and better postnatal management including surgery [3].
It is presumed that one third of patients affected by CDH die in uterus and one third will die in the neonatal period [4]. The standard of care was immediate neonatal surgery followed by postoperative stabilization till the 1980s. Later on, it has been proved that neonatal CDH is a physiological emergency rather than a surgical emergency [5].
The reported incidence of CDH is estimated to be between 1 in 2000 to 5000 births. Defects are more common on the left side, with approximately 80% being left sided and 20% right sided. Bilateral CDH defects are rare and have a high incidence of associated anomalies. Infants with isolated CDH are more likely to be premature, macrosomic and male; and about one third of affected infants may have associated major defects [1].
Structural chromosomal abnormalities have been identified in 9% to 34% of CDH. The cause of CDH is unknown. As with other embryopathies, there is increasing evidence that CDH may be due to the exposure of genetically predisposed or susceptible individuals to environmental factors. Exposure to a number of pharmacologic agents and environmental hazards has been implicated in its development. These include insecticides and drugs, such as phenmetrazine, thalidomide, quinine, cadmium, lead and nitrofen [1]. CDH can be detected during fetal life when screening ultra sonography demonstrates herniation of the intestine and/or the liver into the thorax. Polyhydramnios may lead to antenatal diagnosis in some severe cases.
Neonatal symptoms of CDH are heralded by respiratory distress with insufficient oxygenation, excavated abdomen with sternal protrusion and displacement of the heart sounds to the contra lateral side. In severe cases, APGAR scores at 1 and 5 minutes are low.
Respiratory bruits are absent or decreased on the affected side. Unless energetic treatment is undertaken, respiratory condition deteriorates rapidly until the patient dies. The symptoms of insufficient gas exchange are associated with those of persistent pulmonary hypertension caused by arteriolar constriction and closure of the pulmonary arterial bed that forces maintenance of a pattern of persistent fetal circulation in which the blood from the right ventricle is shunted to the left heart preventing effective gas exchange. In some cases, this pulmonary hypertension intervenes after some hours during which adaptation to a post-natal circulatory pattern with patent pulmonary circulation had taken place. Hypoxia, acidosis, stress or other causes may bring this “honeymoon” period to an end and re-establish the fetal pattern. In some cases without neonatal symptoms, CDH may manifest itself at any age by mild respiratory distress or it can even be an unexpected finding during a medical check-up for other reasons. In these cases, a hernial sac is more often present [3].
Here is congenital diaphragmatic hernia in 6 year old male child presented with symptoms of intermittent chest infection. It is the first case report in Injibara General Hospital, Agaw midir, Ethiopia. Here I am going to stress on delayed presentation of this rare neonatal disease and if happen until child hood expected with hernia sac but in this case with no sac.
Case Report
This is 6year old male child from chagni referred from chagni primary hospital, agaw midir, Ethiopia. He presented with intermittent cough, low grade fever, dyspnea and early satity. He was treated for pulmonary TB years ago and was being treated repeatedly assuming pneumonia. He was admitted in Injibara General Hospital, Agaw Midir, Ethiopia considering Community Acquired Pneumonia (CAP) at pediatrics ward. During admission his Vs was stable except fever of 37.5OC. Chest: decreased air entry on left side. CVS: heard sounds more heard on right side. Abdomen: Scaphoid.
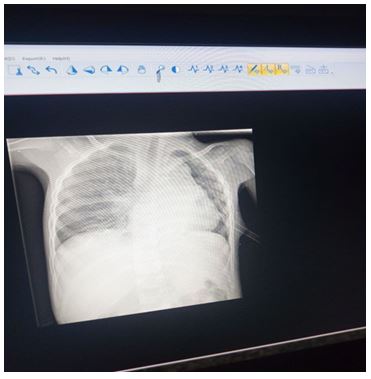
CBC was within normal range. CXR: Reported by radiologist showed, heart pushed to right side, left lung compressed. There was bowel loops within left chest. Conclusion: Congenital diaphragmatic hernia on left side.
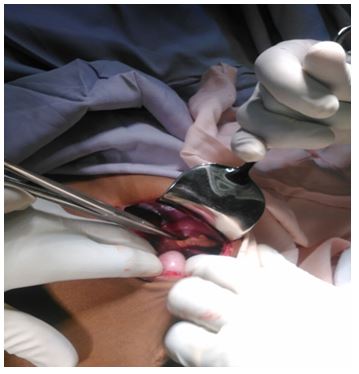
He was transferred after consultation of duty surgeon to surgical ward. Superimposed pneumonia treated for 7 days then semi elective surgery done. Incision was done on left side subcostal incision 8 cm in length. Findings: there was around 8 cm × 4 cm left diaphragmatic defect on poster lateral aspect. The whole small bowel, large bowel except descending colon and below it, spleen was within left chest pushing the mediastinal structures and left lung significantly.
The whole abdominal structures pulled to the abdomen from chest. The diaphragmatic defect repaired using inlay mesh repair technique. Chest tube left in situ. Post operatively the patient was desaturating for that put on intranasal oxygen through concentrator and chest tube output was around 1000 ml. chest tube stayed for one week. Patient discharged stable after 10 days. Post operative chest X-ray showed heart in its natural position well expanded left lung.
Fig.1. Intra operative CDH repair picture.
Fig.2. Pre-operative CXR.
Fig.3. Post-operative CXR.
Discussion
Congenital Diaphragmatic Hernia is rare early neonatal disease condition with incidence of 1 in 3000-5000.
A combination of retrospective and prospective study was done over 12 years from year 2005-2017 G.C. at a tertiary care neonatal referral center in Karnataka, India. Neonates from day 0 to day 30 referred with a clinical suspicion of CDH were included in this study. The diagnosis of CDH was made from chest X-ray and ultra sonography. A total of 83 neonates with CDH were enrolled in this study. Among this, 65/83 (78%) were males and 18/83 (22%) were females with a male to female ratio of 4:1, 75/83 (90%) were left-sided and the remaining were right-sided. The mean hours of life that neonates were admitted was 142 ± 143 h (median 65 h, range 24-765 h) among survivors. Mean onset of respiratory distress in hours was 5.27 ± 1.94 (median 3.5, range 1-12). 45/70 (64%) had nonlethal cardiac malformations. Regarding procedures, 73/83 (88%) underwent various surgical procedures, 10/83 (12%) did not undergo any surgical procedure. In this case series, they operated on six right-sided CDH cases. Of these, five underwent open surgical repair, and in a single case, thoracoscopy was attempted. All are doing well. 67 babies with left-sided CDH underwent various surgical procedures. Of these 63 underwent the open procedure, one required laparoscopic approach, and in another one, the laparoscopic procedure was attempted. Two neonates underwent thoracoscopic repair. Three of them expired postoperatively, one following open surgical repair and another two following open mesh repair.
There were a total of 13/83 (16%) deaths in this study. 8/75 (10.6%) neonates with left-sided CDH died preoperatively and 3/75 (4%) died postoperatively. Whereas 2/8 (25%) neonates with right-sided CDH expired preoperatively. In our study, none of the neonates with right-sided CDH died postoperatively. Overall operative mortality was (3/73) 4.1% [2].
In a research done in Tikuranbessa Specialized Hospital (TASH), which is Ethiopia's largest tertiary referral center and the only pediatric surgical referral hospital in the country, from September 2012-August 2016, twelve cases were included in the study, their ages ranged from 10 hours to 4 years with an average age of 233 days at diagnosis. Only third (33.3%) of the patients were diagnosed during the early neonatal period (before age 7 days). Nine (75%) of our patients presented at our center after 30 days. No patients were diagnosed between 7-30 days of life. Nine patients were males. There were two deaths (mortality=16.6%)
In this study most patients were misdiagnosed and sent to medical centers for the diagnosis of pneumonia. Among them six (50%) were diagnosed with pneumonia and as such were treated first with antibiotics before any imaging was performed. Three (25%) of the 12 patients were diagnosed with neonatal sepsis on presentation.
Only one patient had an initial diagnosis of congenital diaphragmatic hernia within the first 10 hours of life. Four (33.3%) of them had associated congenital abnormalities, including Down Syndrome (DS) (n=2), inguinal hernia (n=1), Sensori Neural Hearing Loss (SNHL) (n=1). One patient had hypospadias and bilateral undescended testes. Average age at surgery was 245 days (range 6 days to 4 years). The most common hernia type was left Bodchalek diagnosed in 5 (41.7%) of cases. All hernias were repaired primarily without mesh. The incisional approach was a subcostal abdominal incision. In the immediate post-operative period, two patients required cardiopulmonary resuscitation. Return of spontaneous circulation was achieved in one patient. One patient suffered from a small bowel obstruction, which was managed conservatively, two months post operatively. One patient developed incisional hernia. One patient was returned to the operating room for jejuno-jejunal intussusceptions requiring exploration and manual reduction. Average length of stay in the hospital was 24.5 days (range 12-60 days). Two of the patients died, making a mortality rate of 16.6% [4]. In a systemic review done in East Carolina, USA, using a MEDLINE search of all clinical reports and a review of articles published between January 1995 and December 2006, using the MeSH search terms ‘diaphragmatic hernia’ and ‘newborns’, included 13 reports from 11 centers. The 13 reports included 763 infants with symptomatic CDH. None of the patients are found at child hood [6].
From the above researches, case reports, systemic review as well as prospective or retrospective studies almost no patient is reported to be at age of child hood. Most patients were presented in early neonatal period tough delayed diagnosis except one case at age of 4yr in tikuranbessa specialized hospital Ethiopia. This case report will give entry to consider diaphragmatic hernia as differential diagnosis of respiratory complaint in child hood as well.
Conclusion
Congenital diaphragmatic hernia is multi factorial congenital abnormalities of early childhood.
It is commonly isolated and most of the time left side posterolateral aspect which is commonly termed as Bochdelk who termed it the first time in medical history of such disease. It is physiologic emergency than medical.
This disease is area of misdiagnosis in medicine. Therefore better to train health professionals working in resource limited health facilities on the diagnosis of CDH.
Since it is one cause of perinatal deaths, pediatricians and gynecologists should be equipped with diagnosis and management of this disease. And it is recommended to take autopsy for those who die with unknown diagnosis in perinatal period though our culture for such practice is low.
This case will give an entry to consider CDH as differential diagnosis in children who presented with respiratory problem.
Acknowledgments
I want to thank the family of this patient to be voluntary for the case to be researched. My great appreciation goes to radiology unit of Injibara General Hospital to peak CDH on CXR. I want to give majestic appreciation for the whole OR and surgical ward team for all activities done to cure this patient. Last not least my gratitude goes to almighty God to give me such courage to conduct researches and register different cases to improve my scientific knowledge despite crowded clinical activities.
References
- Arnold CG. Pediatric surgery, 7th edn. Philadelphia : ELESVIER. 2006; 809-824.
- Gross RE. Congenital hernia of the diaphragm. Am J Dis Child. 1946; 71: 20991991.
- Juan TA. Congenital diaphragmatic hernia. Tovar Orphanet J Rare Dis. 2012; 7: 15.
- Congenital diaphragmatic hernia outcomes in East Africa: The ethiopian experience. Afr J surg. 2016; 21: 3.
- Javaregowda D, Jadhav V, Babu MN, et al. A clinical study on congenital diaphragmatic hernia in neonates: Our institutional experience. J Indian Assoc Pediat Surg. 2018; 23(3):131-139.
- Congenital diaphragmatic hernia: A systematic review and Logan. J Perinatol. 2007; 27:535-549.
Copyright: © 2025 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.