Journal of Medical Sciences and Health Care Research

Research - (2022) Volume 1, Issue 1
Epidemiological Study of Corneal Blindness: A Prospective Observational Study at Sat Kaival Eye Hospital, Sarsa
22Department of Quality Assurance, Sat Kaival College of Pharmacy, Gujarat, India
Received Date: Feb 11, 2022 / Accepted Date: Mar 08, 2022 / Published Date: Mar 15, 2022
Abstract
Objectives: The aim of this study was to determine corneal blindness based on causes, types, occupation, visual acuity and initial drug treatment at sat kaival eye hospital, sarsa.
Materials and methods: I prospectively observed 150 corneal blind patients who came in sat kaival eye hospital Sarsa from January to march 2014. All relative information regarding study was collected by using case proforma. All patients were examined for complete ocular examination, including external eye examination, visual acuity anterior segment examination using slit lamp microscope.
Result and discussion: In this study found that female ratio was higher than to male. More number of patients was in age 50-60. Patients with NO-PLPR were more in numbers. Patients had corneal blindness due to corneal ulcer (39.33%) were higher in compared to other causes. Numbers of patients having unilateral corneal blindness (135) were higher in compared to bilateral corneal blindness (15). Farmer was at high risk of corneal blindness due to their farm work and other chemical that used to spray in farm.
Conclusion: Eye diseases affecting cornea are major causes of corneal blindness. Most of the patients were living in poor condition. They were not educated. Most common cause of corneal blindness was corneal ulcer followed by infectious keratitis. The present study shows more numbers of patients have unilateral corneal blindness. Health promotion strategies are required to be developed. Ocular and personal hygiene plays an important role in reducing the prevalence of corneal blindness.
Keywords
Corneal blindness, Epidemiological study, Visual acuity, Ocular trauma, Corneal ulcer, Infectious keratitis
Abbreviations
WHO: World Health Organization; NPCB: National Programme for Control of Blindness
Introduction
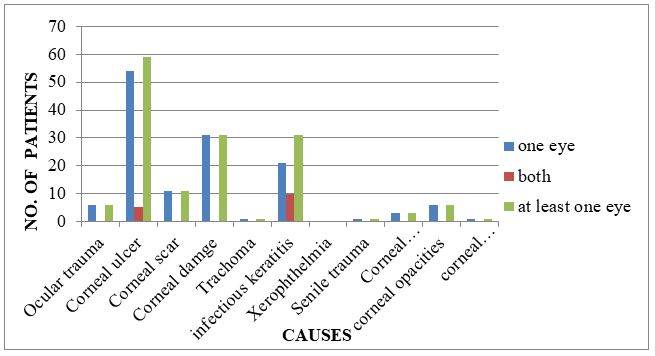
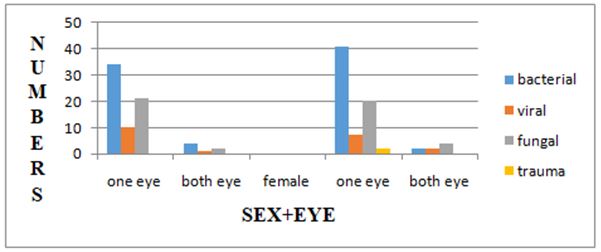
Using the World Health Organization (WHO) definition of blindness as a visual acuity of 3/60 or less [1], it is estimated that currently there are 45 million individuals worldwide who are bilaterally blind and another 135 million that have severely impaired vision in both eyes [2]. The fact that there are 180 million people in the world today who are in some way severely visually disabled is a tragic, unacceptable situation in both social and economic terms, but this number does not even begin to address the additional hundreds of millions who are disabled by monocular visual loss. In recent years the epidemiology of blindness has changed, shifting away from traditional infectious causes, such as trachoma, onchocerciasis, and leprosy, to other important causes, such as cataract (Figure 1) [3]. Indeed, so much emphasis has been placed on managing the backlog of cataract surgery in many developing countries that programmes dealing with other causes of blindness have in some cases been neglected [4].
Fig.1. Causes of corneal blindness in one eye, both eyes and at least in one eye.
According to WHO, it is the fourth major cause of blindness in the world. Its epidemiology is complicated and diverse, and covers a wide range of infectious, inflammatory and degenerative eye diseases. The prevalence of corneal blindness also varies from country to country and even from one population to another, depending upon the availability and general standards of eye care. Currently there are about 37 million bilaterally blind people in the world. Worldwide, major investments in public health infrastructure and primary eye care services have built a strong foundation for preventing future corneal blindness.
All over the world, bacterial keratitis is more common than fungal but this does not hold true for India and other tropical countries. Unlike other parts of our country, hot and humid climatic weather conditions of Kerala favor fungal infections more than bacterial infections. With 7.8 million blind people in India, while 45 million are visually challenged. The country accounts for 20 per cent of the 39 million blind populations across the globe. It is estimated that prevalence of childhood blindness in India is 0.8/1000 children in <16 years age group, implying a total of 300,000 blind children in our country. So a proper understanding of the microbiological and clinical characteristics of the disease will enable the ophthalmologist to initiate appropriate antimicrobial therapy, thereby helping to decrease the incidence of corneal blindness worldwide (From fungal and bacterial keratitis) [5-7].
Corneal blindness is a visual impairment that occurs from cornea becoming clouded, scarred or many other infection that ultimately affect the transparency of cornea, making person blind. Corneal blindness is a common cause of blindness [8]. According to the National Programme for Control of Blindness (NPCB) estimates, there are currently 120,000 corneal blind persons in the country. According to this estimate there is addition of 25,000-30,000 corneal blindness cases every year in the country [5]. The burden of corneal disease in our country is reflected by the fact that 90% of the global cases of ocular trauma and corneal ulceration leading to corneal blindness occur in developing countries [9].
It can affect the person at any age in children, younger, adult or older. Study shows a male preponderance, 60.86% as compared to 39.13% females. This trend is found in various developing countries where men have more chances of accident or trauma due to greater outdoor activity and they have comparatively easier access to health care due to various economic and social factors [5,6]. It affects 1.9 million people (5.1%) globally [10]. The prevalence and causes of corneal blindness vary from one region of the world to another.
First, over half of corneal blindness occurs in children and young adults unlike cataract. Secondly, the best available treatment of corneal blindness is corneal grafting, which is totally dependent on availability of donor corneas [9]. In our country, one of the most important causes for corneal blindness is infective keratitis caused by various infective agents like fungi or bacteria. Depending on the characteristics of population and of geographical areas, there is variation in distribution of causative organisms.
Keratoplasty is the main surgical procedure for the treatment of corneal blindness. There about 150,000 keratoplasties performed in the USA and Europe. India, the country with the largest amount of treatable blindness, performed approximately 17,000 keratoplasties (eye bank Association of India estimate) [11]. Barriers the eye bank services remained under development in myriad region including the lack of trained human resources, inefficient operation, poor distribution infrastructure, high cost of long term storage media, and socio-economic cultural factor associated with organ donation. The lack of tissue is not due to a lack of eye banks, but lack of large professional eye banks that can effectively perform the four key eye bank functions approach, recovery, processing, and distribution [10].
Types of corneal blindness:
1) Bacterial
2) Viral
3) Trauma
4) Nutritional
5) Unilateral
6) Bilateral.
The epidemiology of corneal blindness is divers and highly dependent on the ocular diseases that are endemic in each geographical area. Traditionally, important diseases responsible for corneal blindness include trachoma, onchocerciasis, leprosy, ophthalmia neonatorum and xerophthalmia [11]. Corneal ulcer, corneal damage, corneal disease, trauma, vitamin A deficiency, Infectious keratitis, corneal scar, keratitis scar, with effective public health interventions the incidence of many of these disease showing a declining trend. Cornea become cloudy, scarred, loss of vision may affect one or both eye (Figure 2). Such patient should go undergo an eye and vision examination. The cornea is examined in detail using a slit lamp microscope. Additional tests are sometimes necessary, including topography and keratometry (to study the shape of cornea), pachymetry (to study the thickness of the cornea), specialized microscopy and laboratory studies in some cases.
Fig.2. Patients with corneal blindness.
Objectives
Determination of corneal blindness based on causes, types, and occupation. Determine visual acuity and initial drug treatment.
Rational
By conducting an observational study at Sat Kaival eye hospital Sarsa, the possible causes of corneal blindness were explored by collecting the visual acuity data. These may help to reduce the corneal blindness by treating the patients in initial stages.
Materials and Methods
Source of Data
These study was conducted at Sat Kaival Eye Hospital, Sarsa, Dist-Anand, is situated 12 kilometers away from Anand. This study was conducted for 3 months, from January to March 2014.
Study design: Prospective observational study. Total 150 patients with corneal blindness were observed. In these study, an eye was consider to be corneal blind if the visual acuity in that eye was less than and equal to 3/60 ft. as a results of different corneal disease. All patients were examined for complete ocular examination, including external eye examination, visual acuity anterior segment examination using slit lamp microscope.
Patient’s case proforma was prepared which includes visual acuity of patients at present, age, occupation, sex, numbers of eye affected with corneal different diseases, causes of corneal blindness, type of corneal blindness.
Inclusion criteria:
i) Patients having visual acuity less than and equal to 3/60 ft.
ii) Both unilateral and bilateral corneal blind.
iii) Corneal disease at high risk types.
Exclusion criteria:
i) Patients with ocular hypertonia.
ii) Patients with deteriorated endothelial function.
Statistical Application
The data obtained from patient’s proforma were analyzed for statistical tools using Graph pad prism 5.0 for windows software version 5.03. Chi square test with P-value <0.05 was used to find out significance value of various age groups, sex and occupation.
Results
This present study shows that 150 patients had corneal blindness. Out of 150 patient’s, there were 72(48%) males and 78(52%) were female.
Out of 150 patients who were suffering from corneal blindness, 15 patients had corneal blindness in both eyes while 135 patients had corneal blindness in one eye. Table 1 shows causes of corneal blindness. Corneal ulcer was the leading cause of corneal blindness in at least one eye 59(39.33%) followed by corneal damage and infectious keratitis 31 each (20.66%) in patients who visited hospital. Infectious keratitis was the leading cause of bilateral corneal blindness 10(6.66%).
|
Causes of corneal blindness |
Causes of corneal blindness (no. of patients) |
|||||
|
In one eyes |
In both eye |
In at least one eye |
||||
|
No. |
% |
No. |
% |
No. |
% |
|
|
Ocular trauma |
6 |
4 |
0 |
0 |
6 |
4 |
|
Corneal ulcer |
54 |
36 |
5 |
3.33 |
59 |
39.33 |
|
Corneal scar |
11 |
7.33 |
0 |
0 |
11 |
7.33 |
|
Corneal damage |
31 |
20.66 |
0 |
0 |
31 |
20.66 |
|
Trachoma |
1 |
0.6 |
0 |
0 |
1 |
0.6 |
|
Infectious keratitis |
21 |
14 |
10 |
6.66 |
31 |
20.66 |
|
Xerophthalmia |
0 |
0 |
0 |
0 |
0 |
0 |
|
Senile trauma |
1 |
0.6 |
0 |
0 |
1 |
0.6 |
|
Corneal dystrophies |
3 |
2 |
0 |
0 |
3 |
2 |
|
Corneal opacities |
6 |
4 |
0 |
0 |
6 |
4 |
|
Corneal vascularization |
1 |
0.6 |
0 |
0 |
1 |
0.6 |
|
Total |
135 (90%) |
15 (10%) |
150 (100%) |
|||
Table 1: Causes of corneal blindness in one eye, both eyes and at least in one eye.
Patients with corneal ulcer were more in age group between 51-60 years-26(17.33%). Out of 59 corneal ulcer patients in age group of 51-60 years 55(36.33%) were unilateral corneal blind and 4(2.66%) were bilateral corneal blind (Table 2). Patients having corneal blindness were higher in age group between 61-70 years- 15(10%) followed by corneal damage 11(7.33%) patients (Figure 3).
none
|
Cause of corneal blindness |
Age groups(years) |
|||||||||||||
|
30-40 |
41-50 |
51-60 |
61-70 |
71-80
|
>80 |
Total |
||||||||
|
No |
% |
No |
% |
No |
% |
No |
% |
No |
% |
No |
% |
No |
% |
|
|
Ocular trauma |
0 |
0 |
2 |
1.33 |
2 |
1.33 |
1 |
0.6 |
1 |
0.6 |
1 |
0.6 |
7 |
4.66 |
|
Corneal ulcer |
0 |
0 |
4 |
2.66 |
26 |
17.33 |
23 |
15.3 |
3 |
2 |
3 |
2 |
59 |
39.33 |
|
Corneal scar |
1 |
0.6 |
0 |
0 |
3 |
2 |
6 |
4 |
0 |
0 |
1 |
0.6 |
11 |
7.33 |
|
Corneal damage |
1 |
0.6 |
5 |
3.33 |
13 |
8.66 |
11 |
7.33 |
0 |
0 |
0 |
0 |
31 |
20.33 |
|
Trachoma |
0 |
0 |
0 |
0 |
0 |
0 |
1 |
0.6 |
0 |
0 |
0 |
0 |
1 |
0.6 |
|
Infectious keratitis |
1 |
0.6 |
5 |
3.33 |
7 |
4.66 |
15 |
10 |
2 |
1.33 |
1 |
0.6 |
31 |
20.33 |
|
Xerophthalmia |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
Senile trauma |
0 |
0 |
0 |
0 |
0 |
0 |
1 |
0.6 |
0 |
0 |
0 |
0 |
1 |
0.6 |
|
Corneal dystrophies |
0 |
0 |
2 |
1.33 |
1 |
0.6 |
0 |
0 |
0 |
0 |
0 |
0 |
3 |
2 |
|
Corneal opacities |
2 |
1.33 |
0 |
0 |
3 |
2 |
1 |
0.6 |
0 |
0 |
0 |
0 |
6 |
4 |
|
Corneal vascularization |
0 |
0 |
0 |
0 |
1 |
0.6 |
0 |
|
0 |
0 |
0 |
0 |
1 |
0.6 |
|
Total |
5 |
3.33 |
19 |
12.6 |
58 |
38.66 |
56 |
37.3 |
6 |
4 |
6 |
4 |
150(100%) |
|
Table 2: Causes of corneal blindness in at least one eye for different age groups.
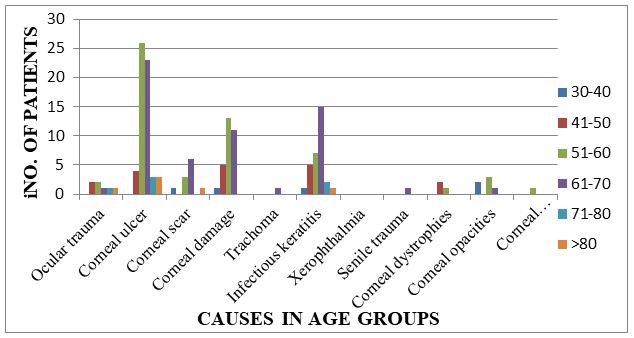
Fig.3. Causes of corneal blindness in at least one eye for different age groups.
Patients with corneal ulcer were more in age group between 51-60 years-26(17.33%). Out of 59 corneal ulcer patients in age group of 51-60 years 55(36.33%) were unilateral corneal blind and 4(2.66%) were bilateral corneal blind (Table 3). Patients having corneal blindness were higher in age group between 61-70 years-15(10%) followed by corneal damage 11(7.33%) patients.
|
Causes of corneal blindness |
Visual acuity |
|||||||||||||||
|
No PLPR |
1/2 ft |
1 ft |
11/2 ft |
2 ft |
21/2 ft |
3ft |
Total |
|||||||||
|
No |
% |
No |
% |
No |
% |
No |
% |
No |
% |
No |
% |
No |
% |
No |
% |
|
|
Ocular |
2 |
1.33 |
1 |
0.6 |
0 |
0 |
0 |
0 |
1 |
0.6 |
0 |
0 |
1 |
0.6 |
6 |
3 |
|
Corneal |
27 |
18 |
13 |
8.6 |
9 |
6 |
3 |
2 |
5 |
3.3 |
0 |
0 |
2 |
1.3 |
59 |
39.3 |
|
Corneal |
0 |
0 |
4 |
2.6 |
3 |
2 |
0 |
0 |
3 |
2 |
1 |
0.6 |
0 |
0 |
11 |
7.33 |
|
Corneal damage |
12 |
8 |
8 |
5.33 |
2 |
1.6 |
0 |
0 |
6 |
4 |
0 |
0 |
3 |
2 |
31 |
20.6 |
|
Trachoma |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
1 |
0.6 |
0 |
0 |
1 |
0.6 |
|
Infectious keratitis |
10 |
6.6 |
8 |
5.33 |
2 |
1.6 |
0 |
0 |
4 |
2.6 |
0 |
0 |
7 |
4.66 |
31 |
20.6 |
|
Xerophthalmia |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
Senile |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
1 |
0.6 |
1 |
0.6 |
|
Corneal dystrophies |
2 |
1.3 |
0 |
0 |
1 |
0.6 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
3 |
2 |
|
Corneal opacities |
2 |
1.3 |
2 |
1.3 |
1 |
0.6 |
0 |
0 |
1 |
0.6 |
0 |
0 |
0 |
0 |
6 |
4 |
|
Corneal |
1 |
0.6 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
1 |
0.6 |
|
Total |
56 |
36 |
18 |
3 |
20 |
2 |
14 |
150 |
||||||||
Table 3: Causes of corneal blindness in at least one eye based on visual acuity.
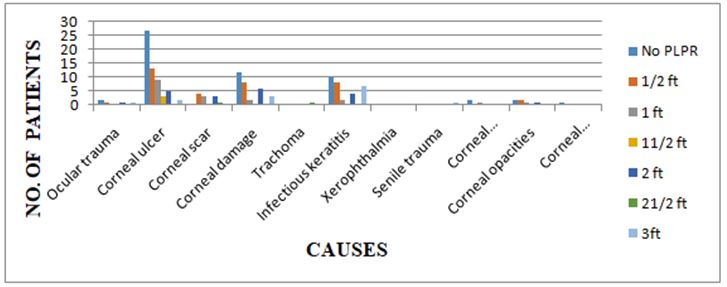
Figure 4 shows the distribution of visual acuity in 150 patients with corneal blindness based on the causes of corneal blindness. The majority of eyes with corneal blindness caused by corneal ulcer, infectious keratitis and corneal damage in elder people due to their out-door work, with the highest proportion of eyes had NO-PLPR.
A total of 165 eyes suffered from corneal blindness, which includes 135 eyes of 135 patients who had corneal blindness in one eye and 30 eyes of 15 patients who had corneal blindness in both eyes. Out of 150 patients 56 patients had visual acuity of NO-PLPR.
Fig.4. Distribution of visual acuity of 150 patients with corneal blindness based on causes of corneal blindness. Total represents all eyes blind due to corneal disease.
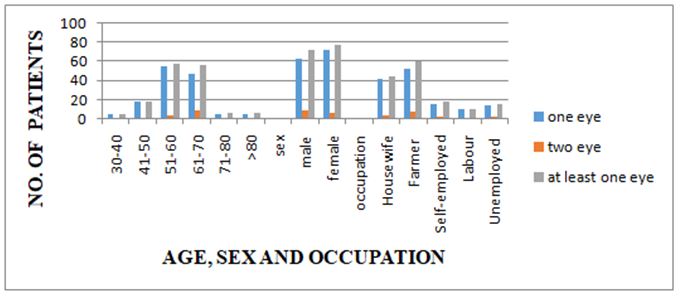
Table 4 shows the age, sex and occupation wise distribution of corneal blindness in one eye, both eyes and at least in one eye. Out of total 150 corneal blind patients more numbers of patients were females 78(52%) and 72(48%) males having corneal blindness at least in one eye
(Figure 5). Based on occupation farmers were more in numbers-60(40%). Out of 60 farmers, 52(34.66%) were having corneal blindness in one eye and 8 (5.33%) were having corneal blindness in both eyes. Out of 45 female patients- 42(28%) were unilateral and 3(2%) were bilateral corneal blind (P-value <0.0001).
Fig.5. Distribution of corneal blindness by age, sex and occupation.
|
|
Corneal blindness |
|
|||||
|
Age groups (years) |
One eye |
Both eyes |
At least one eye |
|
|||
|
NO (135) |
% |
NO (15) |
% |
NO (150)
|
% |
|
|
|
30-40 |
5 |
3.33 |
0 |
0 |
5 |
3.33 |
|
|
41-50 |
18 |
12 |
1 |
0.6 |
19 |
12.66 |
|
|
51-60 |
55 |
36.66 |
4 |
2 |
59 |
38.66 |
|
|
61-70 |
47 |
31.33 |
9 |
6 |
56 |
37.33 |
|
|
71-80 |
5 |
3.33 |
1 |
0.6 |
6 |
3.99 |
|
|
>80 |
5 |
3.33 |
1 |
0.6 |
6 |
3.99 |
|
|
Sex |
|
|
|
|
|
|
|
|
Male |
63 |
42 |
9 |
6 |
72 |
48 |
|
|
Female |
72 |
48 |
6 |
4 |
78 |
52 |
|
|
Occupation |
|
||||||
|
Housewife |
42 |
28 |
3 |
2 |
45 |
30 |
|
|
Farmer |
52 |
34.66 |
8 |
5.33 |
60 |
39.99 |
|
|
Self-employed |
16 |
10.66 |
2 |
1.33 |
18 |
11.99 |
|
|
Labour |
11 |
7.33 |
0 |
0 |
11 |
7.33 |
|
|
Unemployed |
14 |
9.33 |
2 |
1.33 |
16 |
10.99 |
|
Table 4: Distribution of corneal blindness by age, sex and occupation.
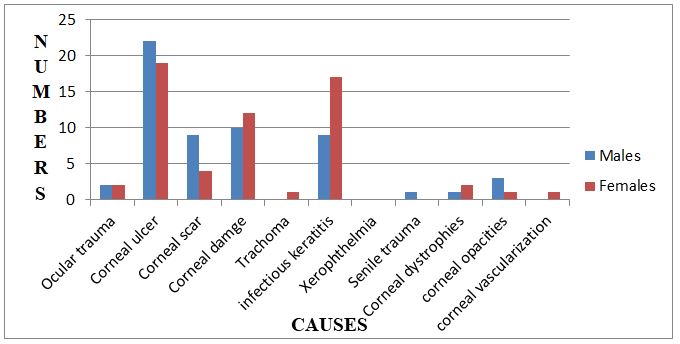
This study shows that corneal ulcer was more common in males 35(22.6%) and females 24(16%) total 59, followed by infectious keratitis and corneal damage total 31(20.33%) each (Table 5). Corneal scar and trauma leading to corneal blindness occurred while playing in out –door (Figure 6).
|
Cause |
Males (n=135) No% |
Female (n=15) No% |
Total (n=150) No% |
|||
|
Ocular trauma |
3 |
2 |
2 |
1.33 |
5 |
3.33 |
|
Corneal ulcer |
35 |
22.6 |
24 |
16 |
59 |
39.33 |
|
Corneal scar |
3 |
2 |
8 |
5.33 |
11 |
7.33 |
|
Corneal damage |
14 |
9.33 |
17 |
11.33 |
31 |
20.33 |
|
Trachoma |
0 |
0 |
1 |
0.6 |
1 |
0.6 |
|
Infectious keratitis |
11 |
7.33 |
20 |
14 |
31 |
20.33 |
|
Xerophthalmia |
0 |
0 |
0 |
0 |
0 |
0 |
|
Senile trauma |
1 |
0.6 |
0 |
0 |
1 |
0.6 |
|
Corneal dystrophies |
1 |
0.6 |
2 |
1.33 |
3 |
2 |
|
Corneal opacities |
5 |
3.33 |
2 |
1.33 |
7 |
4.2 |
|
Corneal vascularization |
0 |
0 |
1 |
0.6 |
1 |
0.6 |
|
Total |
72 (48%) |
78 (52%) |
150 (100%) |
|||
Table 5: Causes of corneal blindness in at least one eye based on sex groups.
none
Fig.6. Causes of corneal blindness in at least one eye based on sex groups.
This study shows that corneal ulcer was more common in males 35(22.6%) and females 24(16%) total 59, followed by infectious keratitis and corneal damage total 31(20.33%) each. Corneal scar and trauma leading to corneal blindness occurred while playing in out-door.
Table 6 shows that more number of male and female with corneal blindness in one and both eyes. More number of females (70) was having unilateral corneal blindness in compared to males (65) patient. Patients with bilateral corneal blindness were 7 and 8 in male and female respectively. Patients with bacterial type of infection were higher in both male and females in compared to other infections (Figure 7). Total 43 females were having bacterial infection in compared to 38 males. Viral infection was more in males (11-patients) in compared to females (9- patients). Patients with bilateral corneal blindness due to bacterial and fungal infection were similar in male (7) and female (7).
|
Types |
MALE |
FEMALE |
||||||
|
One eye |
Both eye |
One eye |
Both eye |
|||||
|
No. |
% |
No |
% |
No |
% |
No |
% |
|
|
Bacteria |
34 |
22.66 |
4 |
2.66 |
41 |
27.33 |
2 |
1.33 |
|
Viral |
10 |
6.66 |
1 |
0.6 |
7 |
4.66 |
2 |
1.33 |
|
Fungal |
21 |
14 |
2 |
1.33 |
20 |
13.33 |
4 |
2.66 |
|
Trauma |
0 |
0 |
0 |
0 |
2 |
1.33 |
0 |
0 |
|
Total |
65 |
43.33 |
7 |
4.6 |
70 |
46.66 |
8 |
5.33 |
Table 6: Distribution of corneal blindness based on types in male and female.
Fig.7. Distributions of corneal blindness based on types in male and female.
Management of corneal blindness condition
Drugs prescribed for initial treatment (Figures 8-11).
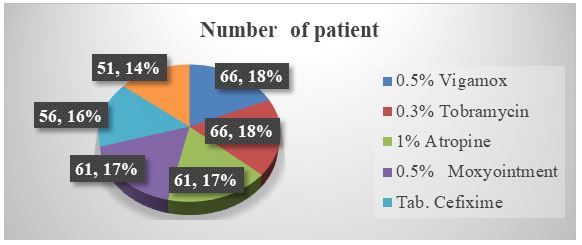
Fig.8. Antibacterial.
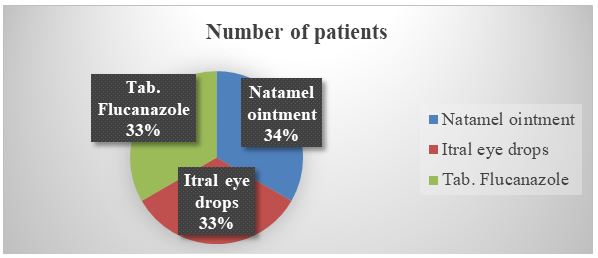
Fig.9. Antifungal.
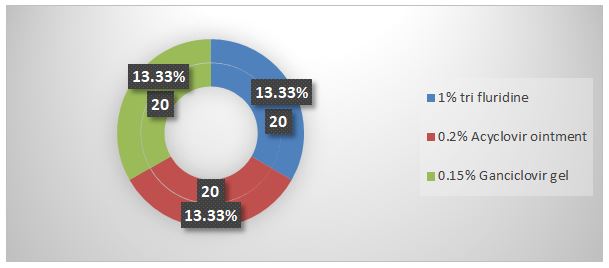
Fig 10. Antiviral.
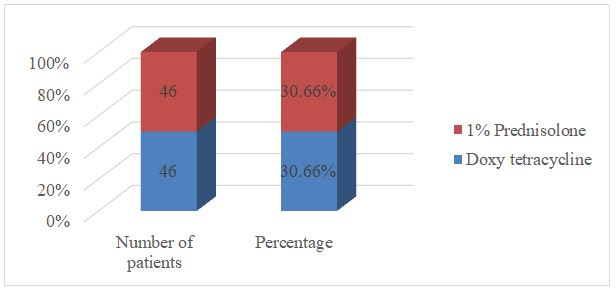
Fig.11. Antibiotic.
Discussion
This recent study provided information about patients having corneal blindness in Sat Kaival eye hospital. This could assist in developing strategies to reduce corneal blindness in surrounding areas. These population based data on the causes of corneal blindness suggested that 150 patients (from January to March 2014) had corneal blindness due to various causes that affecting cornea. Patients having corneal blind eye with unilateral and bilateral corneal blindness were respectively 90% and 10%. The presence of corneal blindness varies between different age groups, sex wise, and causes wise. Patients with corneal blindness increase with increase in age being, maximum in age between 51-60 years (38.66%).
Out of total 150 patients who had visited the hospital 42% were males and 48% were females having corneal blindness. Number of corneal blind patients in farmers (34.66%) was higher due to their exposure to vegetative matter like thorns, branches, plants secretion. Number of corneal blind was lowest in labor 0.44%. Patients in other categories like self employed and unemployed were lower in numbers. In labors the reason for corneal blindness might be tools and due to lack of awareness regarding occupational hazards. A total 165 eyes suffered from corneal blindness, which includes 30 eyes from 15 patients who had corneal blindness in both eyes and 135 eyes of 135 patients who had corneal blindness in one eye.
Corneal ulcer was the leading cause of corneal blindness in this study. Corneal damage and infectious keratitis were 2nd leading causes of corneal blindness. Males have been reported to have higher chances of corneal ulcer. These might be due to more out-door activity of males in compared to females. Patients having corneal blindness were more in age between 51-60 years. Senile trauma and trachoma were observed in 1-1 patient each.
Conclusion
Most common cause of corneal blindness was corneal ulcer followed by infectious keratitis. More numbers of patients’ were farmers because there were chances of damage to cornea due to vegetative matter were higher. Incidence of corneal blindness was more in elder age patients. 150 patients of corneal blindness in at least one eye nearly 45% of this blindness is avoidable. The avoidable causes of corneal blindness include keratitis, corneal scar, and corneal opacities. The need for decreasing corneal blindness in long term with effective health promotion strategies is very important. Health promotion programs to reduce corneal blindness need to target those who are at higher risk of suffering from corneal blindness based on the study. The major causes of corneal blindness based on this study data that need attention are corneal ulcer and infectious keratitis in elders. Safety at work places has to be improved to reduce trauma causing corneal blindness. Requirements for appropriate eye protection for people performing high risk work can reduce risk of corneal blindness. There is significant burden of corneal blindness in this population based study, encompassing a variety of corneal infection, majority of which are avoidable. Health promotion strategies have to be developed and implemented to raise awareness about the causes and prevention of corneal blindness.
References
- Resnikoff S,Pascolini D, Etya’ale D. Global data on visual impairment blindness in the year 2002. Bull World Health Organ. 2004; 82(11):844-851.
- Whitcher JP, Srinivasan M. Corneal blindness: A global perspective. Bull WHO. 2001; 79:214-221.
- Jenchitr W. Corneal blindness. Thai J Ophthalmol. 1990; 4:155-161.
- Upadhyay MP, Karmacharaya PC, Koirala S. Epidemiological characteristics, predisposing factors and etiological diagnosis of corneal ulceration in Nepal. Am J Ophthalmol. 1991;111:92-99.
- Gonzales CA, Srinivasan M, Whitcher JP. Incidence of Corneal ulceration in Madurai district, SouthIndia. Ophthal epidemiol.1996; 3159-3166.
- Upadhyaya MP, Srinivasan M. Corneal blindness: A global perspective. Bull WHO. 2001; 79:214-221.
- Oliva MS, Gulati M, Schottman T. Turning the tide of corneal blindness. Indian J Ophthalmol. 2012; 149:425.
- Frederick S. Corneal surgery: Theory, technique and tissue. Elsevie Health Sci. 2008; 684.
- Yanoff M, Jay S, Duker, James J, et al. In Ophthalmology; 3rd Edn. Elsevier Health Sciences. 2009.
- Dandona R, Dandona L. Corneal blindness in southern Indian population and for Health promotion strategies. Br J Ophthalmol. 2003; 87:133-141.
- Dandona L, Dandona R, Naduvilath TJ. Is current eye-care-policy focus almost exclusively on cataract adequate to deal with blindness in India. Lancet. 1998; 351:1312-1316.
Copyright: © 2025 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.