Nanomedicine and Nanoscience Technology: Open Access

Review - (2021) Volume 1, Issue 1
Nano Aerogels an Aerosolised Gel Therapy
Received Date: Sep 28, 2021 / Accepted Date: Nov 02, 2021 / Published Date: Nov 10, 2021
Abstract
Administration of medications via aerosolization with gels is potentially an ideal strategy to treat airway diseases. This delivery method ensures high concentrations of the medication in the targeted tissues, the airways, with generally lower systemic absorption and systemic adverse effects. Aerosolized antibiotics have been tested as treatment for bacterial infections and viral infections in patients with Cystic Fibrosis (CF), Non Cystic Fibrosis Bronchiectasis (NCFB), pneumonia, Coronary Obstructive Pulmonary Disorder (COPD) and Ventilator-Associated Pneumonia (VAP). The most successful application is the treatment of infections in patients with CF. It has been hypothesized that similar success would be seen in NCFB. This review summarizes the available evidence supporting the use of aerosolized antibiotics in many bacterial and viral infections to potentiate immediate release of drug at targeted site and also may shows effective results on corona virus in futuristic view.
Keywords
Pneumonia, Nano aerogels, Nano particles, Aerosolization, Bronchodilators, Steroids
Abbreviations
Computational Cystic Fibrosis (CF); Non Cystic Fibrosis Bronchiectasis (NCFB); Coronary Obstructive Pulmonary Disorder (COPD); pressurized Metered Dose Inhalers (pMDIs); Dry Powder Inhalers (DPIs); Ventilator Associated Pneumonia (VAP); Mass Median Aerodynamic Diameter (MMAD); Nasal-Associated Lymphoid Tissue (NALT); Soy Phosphatidylcholine (SPC); Phospholipid Dimyristoyl Phosphatidylglycerol (DMPG); Trimethyl Chitosan (TMC); Metered Dose Inhalers (pMDIs); Dry Powder Inhalers (DPIs); Soft-Mist Inhalers (SMIs); Fine Particle Fraction (FPF); Emitted Dose (ED)
Introduction
The delivery of medications to the lungs via inhalation or aerosolization has long been recognized as a technique to ensure high local drug concentration with minimal systemic side effects. This mode of therapy is used successfully to deliver bronchodilators, steroids to patients with asthma and COPD and is potentially a compelling strategy to target respiratory tract infections. The most successful application in this strategy in the treatment of infections in patients with Cystic Fibrosis (CF). It has been hypothesized that similar efficacy would be seen in patients with Non Cystic Fibrosis Bronchiectasis (NCFB) and in difficult to treat hospital acquired infections such as Ventilator Associated Pneumonia (VAP). This review summarizes the most relevant evidence regarding the use of aerosolized antibiotics in patients with CF, NCFB, and VAP. Additionally by further advanced research aerosolized gelation of polymeric drug nanoparticles by nanotechnology shows promising immediate results by the targeted site of action and extended release of drug especially an optional trial for corona virus.
Systemic delivery of drugs through inhalation (oral and nasal) is an attractive alternative for oral or parenteral drug delivery. Drug delivery to lungs through inhalation has advantages such as high bioavailability, rapid onset of action due to its large surface area for absorption, self-administration, improved patient compliance, non-invasive nature, limited drug degradation, and high solute permeability. Pulmonary route has been used for local delivery of drugs like antibiotic, protein, peptide, chemotherapeutics, interferon, antitrypsin, protease inhibitors, deoxyribonucleases, vaccines and many more. An important consideration in pulmonary delivery is aerosolization of the drug. Delivery of drug to the lungs has to go through physical obstruction and physiological obstruction which includes the multiple bifurcation of respiratory tract and the innate immunological response. However, inhalation is not new, inhaled fumigation was known in the first century and antiseptic aerosol therapy was popular in mid-20th century. Particles deposit in the respiratory track by virtue of their size, shape and surface properties. There are three main mechanisms by which particles deposit in respiratory tract: impaction, sedimentation and/or diffusion. Particles deposit in the mid and deep lung regions when the aerodynamic particle size is ≤ 5 μm, which is where nanoparticles have a niche in advanced pulmonary drug delivery. Nanoparticles can be used for targeted delivery, sustained delivery and deep lung delivery of drugs and therapeutics. A recent term, “nanoperiodic property”, has been introduced by Kannan et al. which relates nanoparticle behavior to its in vivo behavior. Particle size, shape, surface chemistry, flexibility/rigidity, architecture and elemental composition have been identified as “critical nanoscale.
Inhalable Powders for Lung Delivery
Particle deposition in the lung depends predominantly on its properties including particle size, size distribution, particle morphology, surface morphology, hygroscopicity, electrical charge and density. Other factors include the diseased state and breathing pattern. The geometric diameter of a particle is less influential than aerodynamic diameter. Hence, the United States Pharmacopeia (USP) Chapter b 601 N defines Mass Median Aerodynamic Diameter (MMAD). MMAD means that 50% of particles in the aerodynamic size distribution, based on mass, lie above and below that diameter. Larger particles deposit in the airway due to inertial impaction and sedimentation while smaller particles deposit by diffusion ciliated columnar epithelium in the upper airway secretes mucus which is a thick gel layer [1-4]. The primary function of the mucosal layer is to protect the lungs by trapping and removing foreign particles by the mucociliary escalator which causes trapped particles to be coughed up out of the lungs. Particles reaching the deep lung alveolar region may be susceptible to clearance by alveolar macrophages by phagocytosis depending on the surface chemistry of the particles. To evade mucociliary trapping and clearance, the inhaled particle should either be of small size to be inhaled past the upper lung region or have the appropriate surface chemistry to avoid adhesion to the mucosal layer and/or mucopentration [5-11]. Use of hydrophilic and neutrally charged polymers helps in escaping mucus adhesion. Lung phagocytosis can be significant for particles of geometric diameter (dg) 1 μm ≤ dg ≥ 2 μm, dependent on the surface chemistry of the particles, and decreases for particles smaller and larger. Dense surface charge and low molecular weight PEGylated nanoparticles can penetrate the mucus.
Infected airways have compromised mucociliary clearance and are vulnerable to bacterial biofilm formation, which is highly resistant to antibiotics and requires additional dose through conventional routes of administration. Inhalation of antibiotic for pulmonary infection has been proven clinically to be more effective than other routes of administration. Nanoparticles in the size range of 200 nm are effective in mucus penetration. Creating nanoparticles to exhibit biphasic release profile will give high initial burst followed by sustained release of antibiotic to maintain sufficient drug concentration to inhibit bio film growth. Additionally PEGylated liposomal formulations have proved to be effective in mucus penetration and escaping pulmonary and immune clearance.
Nasal Delivery of Nanoparticles
Nasal route is a choice for vaccine delivery due to ease of delivery through nose, high vascularity in nose, large surface area for absorption and low enzymatic degradation. Inhalable powder formulations for nasal delivery enhance systemic bioavailability and are superior to liquid formulations. Advantages of dry powders also include increased chemical stability, no requirement for preservatives, and feasibility of administering relatively large amounts of drug. Improved nasal delivery of vaccines through nanoparticles may be effective at promoting improved uptake of particles by the Nasal-Associated Lymphoid Tissue (NALT) system. Nanoparticles larger than 20 nm will cross mucosal membranes through the transmucosal route using endocytosis, carrier-mediated or receptor-mediated transport processes. There is no significant difference in immune response between nano and microparticles [12].
Mucoadhesion is key to nasal delivery of drugs. Chen et al formulated liposomes of bovine serum albumin coated with polymer to increase bioavailability and mucoadhesion. The liposomes were made of Soy Phosphatidylcholine (SPC) and Phospholipid Dimyristoyl Phosphatidylglycerol (DMPG) coated with alginate, chitosan or Trimethyl Chitosan (TMC). Polymer coating resulted in increased size of liposome [13-20]. However, mucoadhesion property of chitosan and TMC particles increased compared to alginate coated and uncoated particles. Dehghan et al formulated a polymeric nanosphere nasal vaccine for influenza which enters the body through the inhalation route. In the study, they prepared dry nanoparticle powders of influenza vaccines with two other immunoadjuvants using chitosan as the carrier. The formulation demonstrated that the vaccine structure and characteristics of chitosan did not change after the formulation. The particles had a size of 581.1 ± 32.6 nm with mucoadhesive properties of chitosan that makes it suitable for nasal delivery of vaccine. Dry powder chitosan nanospheres may be an appropriate delivery system for nasal immunization of influenza, due to the nano size range, the ability for chitosan to adhere to mucosal membranes, and suitable release profile. Another study on nasal vaccine delivery was conducted by Wang et al where they formulated anthrax vaccine for dry powder nasal delivery. Vaccination at the site of entry can be more effective than the systemic route, simply because the pathogens can be encountered and neutralized at entry before it gets into the systemic circulation. The nasal route is preferred for its mucous layer, hence nasal products should be mucoadhesive. Inhalable nasal powders are gaining popularity as new vaccine delivery by virtue of their stability compared to liquid formulations that require refrigeration or preservatives. A report by Wang et al investigated a nasal formulation composed of recombinant protective antigen, compound 48/80 mast cell activator as a mucosal adjuvant, and trehalose. The particle size was ~ 25 μm and the vaccine maintained its structural integrity throughout processing. In vivo study of the formulation, in rabbits showed the vaccines competence to neutralize anthrax lethal toxin. They also found that the dry powder vaccine was effective even after 2.5 years of storage at room temperature which will alleviate the cold chain shipping problem for vaccine. An in-situ gel forming dry powder formulation was developed by Velasquez et al using norovirus like particles with mucoadhesive polymer GelSite®. In vivo study of the formulation showed that the vaccine induced higher antigen response than liquid preparation [21-28].
The overall anatomy and physiology of the pulmonary system are complicated and the dynamic pulmonary clearance mechanisms present challenges for drug delivery through this route. Despite these potential challenges, there are four clinically successful pulmonary inhalation pharmaceutical dosage forms based on device classes; namely, nebulizers (nebs), pressurized Metered Dose Inhalers (pMDIs), Dry Powder Inhalers (DPIs), and Soft-Mist Inhalers (SMIs). Nebulizers produce liquid aerosols by an external power supply and do not contain any propellant unlike pMDIs. Nebulizers require an external power source and owing to its size is restricted to clinical settings and in-house use for niche patient populations (i.e. young children and the elderly), while pMDI offers portability and patient convenience. However, propellant effects on the environment, solubility and compatibility challenges of drug with propellant and physicohemical stability challenges are common. DPIs can contain respirable powdered drug or respirable powdered drug blended with a non-respirable carrier. There are many unique advantages of DPIs. Powdered drug offers an advantage especially for delivery of poorly water-soluble drug, and protein and peptide drugs which cannot withstand the shear generated during inhalation.
DPI is a rapidly growing sector of the pulmonary inhalation pharmaceutical market which is evident by the increasing number of successful products in the market. Recent FDA approval of Afrezza®, the inhaled insulin will invite more research and growth into inhalation therapy. DPIs can have two potential problems concerning relatively low Fine Particle Fraction (FPF) and Emitted Dose (ED) which can be attributed to insufficient particle dispersion by the patient or DPI device, aerosol dispersion inefficiency, or the powder formulation itself. FPF is the fraction of inhaled particles that are smaller than a certain aerodynamic diameter, and ED is the proportion of initial dose that is delivered out of the device, as described in USP Chapter b 601 N. The emerging technologies in overcoming these problems will be discussed in detail in this article [29].
TABLE 1: Drug class, condition and route of administration.
Hollow Nanoparticles and Nanoaggregates
Formulating nanoparticles into large hollow or porous particles increases the geometric diameter and decreases aerodynamic diameter of particles, thereby making the particle more suitable to deposit in the lung. Geometric diameter of a particle contributes less to particle deposition while aerodynamic diameter determines the deep lung deposition of nanoparticles. Large particles can be improved to behave like small particles [30]. A study conducted by Edward et al demonstrated that porous particles with drug have higher aerosolization efficiency, sustained release and increased bioavailability.
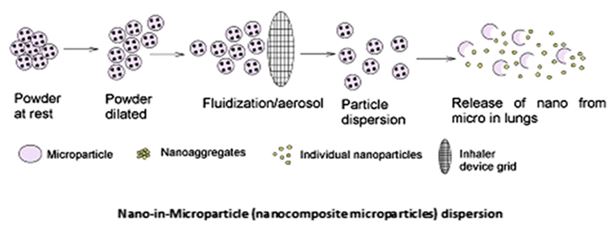
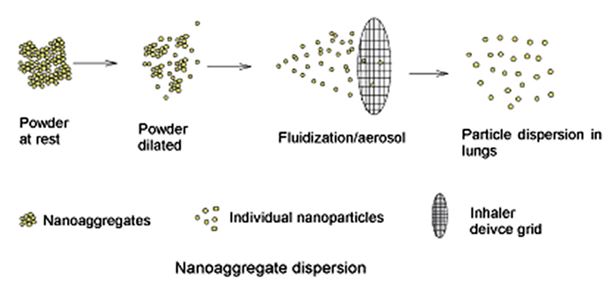
Nanoparticle aggregates are drug containing nanoparticles accumulated together, which may dissociate into individual nanoparticle and release the drug in the lungs or respiratory tract large hollow nanoparticulate aggregates which possess geometric diameter ~ 10 μm exhibit a small aerodynamic diameter (1-5 μm) due to low particle density. The larger particles reduce the tendency for the particles to aggregate in the inhaler device which will ensure proper delivery of the powder while the smaller particle will avoid deposition elsewhere in the respiratory tract but the lungs [31].
FIG. 1.Schematic of the dispersion mechanism for inhalable nanoparticles as aerosolized dry powders containing non-respirable carrier particles.
FIG.2. Schematic of the dispersion mechanism for inhalable nanoparticles as aerosolized dry powders as carrier-free respirable particles.
Conclusion
Inhalable nanoparticles in the solid-state as inhalable powders for targeted pulmonary delivery offer unique advantages and are a new area of research. However, there are limitations. Toxicity of nanoparticles (i.e. nanotoxicity), polymers and other excipients is critical for the development of safe inhalable dry powder inhalation formulations. Nasal delivery of inhalable nanoparticulate powders is gaining research attention recently, particularly in vaccine applications for corona virus, systemic drug delivery in the treatment of pain, and non-invasive brain targeting. Surface modification and formulation optimization can improve nanoparticle stability, dispersion, and deep lung deposition. Various pharmaceutical processing methods can be employed including advanced spray drying, spray freeze drying, milling, supercritical fluid extraction, condensation aerosol growth, thermal condensation and the main aim of this review is that aerosolized gel therapy is very selective option to treat immediately spreadable bacterial, viral infections such as corona virus.
References
- Stockininn C, Robei ts JK, Ye llepeddi VK, et al. Clinical pharmacokinetics of inhaled antimicrobials. Clin Pharm. 2015; 54(S):473-492.
- Hochhaus G, Horhota S, Hendeles L, et al. Phariacokinetics of orally inhaled drug products. AAPS J 2015; 17(3):769-775.
- Yang JW, Fan LC, Lu HW, et al. Efficacy and safety of long-term inhaled antibiotic for patients with noncystic fibrosis bronchiectasis: A meta-analysis. Clin Respir J. 2015; 10(6):731-739.
- Konstan MW, Geller DE, Minic P, et al. Tobramycin inhalation powder manufactured by improved process in cystic fibrosis: The randomized EDIT trial. Pediatr Pulinonol. 2011; 46(3):230-238.
- Konstan MW, Fltime PA. Kappler M, et al. Safety, efficacy and convenience of tobramycin inhalation powder in cystic fibrosis patients: The EAGER trial. J Cyst Fibros. 2011: 10:54-61.
- Stephens D, Garey N, Isles A, et al. Efficacy of inhaled tobramycin in the treatment of pulmonary exacerbations in children with cystic fibrosis. Pediatr Infect Dis. 1983; 2:209-211.
- Le Brun PP, Vinks AA, Touw DJ, et al. Can Tobramycin inhalation be improved with a jet nebulizer? Ther Drug Monit. 1999: 21:615-624.
- Geller DE, Konstan MW, Smith J, t al. Novel tobramycin inhalation powder in cystic fibrosis subjects: Pharmacokinetics and safety. Pediatr Pulinonol. 2007; 42:307-313.
- Hoffmann IM, Rubin BK, lskandar SS, et al. Acute renal failure in cystic fibrosis: Association with inhaled tobraimycin therapy. Pediatr Pulmonol. 2002; 34:375-377.
- Gibson RL, Retsch-Bogart GZ, Oermann C, et al. Microbiology, safety and pharmacokinetics of aztreonam lysinate for inhalation in patients with cystic fibrosis. Pediatr Puliaatinol. 2O06; 41:656-665.
- Falagas ME, Sieinpos II, Bliziotis IA, et al. Administration of antibiotics via the respiratory tract for the prevention of ICU-acquired pneumonia: A meta-analysis of comparative trials. Crit Care 2006; 10:R123.
- Kollef MH. Hamilton CW, Montgomery AB. Aerosolized antibiotics: Do they add to the treatment of pneumonia? Curr Opin Infect Dis. 2013; 26:535-544.
- Ilowite JS, Gorvoy JD, Sinaldone GC. Quantitative deposition of aerosolized gentamicin in cystic fibrosis. Ans Rev Respir Dis. 1987; 136: 1445-1449.
- Miller DD, Pal mer LB, Shah AR, et al. Aerosol delivery and modern mechanical ventilation: In vitro/in vivo evaluation. Am J Respir Crit Care Med. 2003; 168:1205-1209.
- Niederman MS, Chastre I, Corkery K, et al. BAY41-6551 achieves bactericidal tracheal aspirate amikacin concentrations in mechanically ventilated patients with Gram-negative pneumonia. Intensive Care Med. 2012; 38: 263-271.
- Ferrari F, Liu ZH, Lu Q, et al. Comparison of lungs tissue concentrations of nebulized ceftazidime in ventilated piglets: Ultrasonic versus vibrating plate nebulizers. Intensive Care Med. 2008; 34: 1715-1723.
- Chalmers JD, Smith MP, McHugh BJ, et al. Short and long-term antibiotic treatment reduces airway and systemic inflammation in non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med. 2012; 186: 657-665.
- Zampieri FG, Nassar AP Jr, Gusmao-Flores D, et al. Nebulized antibiotics for ventilator associated pneumonia: A systematic review and meta-analysis. Crit Care. 2015: 19:1-50.
- Kannan RM, Nance E, Kannan S, et al. Emerging concepts in dendrimer-based nanomedicine: From design principles to clinical applications. J Intern Med. 2014; 276:579-617.
- Garcia A, Mack P, Williams S, et al. Microfabricated engineered particle systems for respiratory drug delivery and other pharmaceutical applications. J Drug Deliv. 2012; 10:941243.
- Mandell LA, Wunderink RG, Anzueto A, et al. Infectious diseases society of America/American thoracic society consensus guidelines on the management of community acquired pneumonia in adults. Clin Infect Dis. 2007; 44:527-S72.
- Dhariwal AK, Tullu MS. Colistin: Re-emergence of the ‘forgotten’ antimicrobial agent. Int Postgrad Med. 2013; 59:208-215.
- Lu Q, Yang J, Liu Z, Gutierrez C, et al. Nebulized ceftazidime and amikacin in ventilator-associated pneumonia caused by Pseudomonas aeruginosa. Am I Respir Crit Care Med. 2011; l84:106-115.
- Palmer LB, Smaldone GC, Chen JJ, Baram D, et a1. Aerosolized antibiotics and ventilator associated tracheabronchitis in the intensive care unit. Crit Care Med. 2008; 36:2008-2013.
- Wood GC. Aerosolized antibiotics for treating hospital-acquired and ventilator-associated pneumonia. Expert Rev Anti Infect Ther. 2011; 9:993-1000.
- Edson RS, Brey RH, Me Donald TJ, et al. Vestibular toxicity due to inhaled tobramycin in patient with renal insufficiency. Mayo Clin Proc. 2004: 79:1185-1191.
- Rubin BK. Aerosolized antibiotics for non-cystic fibrosis broncliectasis. J Aerosol Med Pulm Drug Deliv. 2008; 21:71-76.
- Prober CG, Watson PD, Jones J. Technical report: Precautions regarding the use of aerosolized antibiotics. Pediatrics. 2000; 106: E89.
- Palmer LB, S maldone GC. Reduction of bacterial resistance with inhaled antibiotics in the intensive care unit. Am J Respir Crit Care Med. 2014; 189:1225-1233
- Alothman GA, Alsaadi MM, Ho BL, et al. Evaluation of bronchial constriction in children with cystic fibrosis after inhaling two different preparations of tobrainycin. Chest. 2002; 122:930-934.
- Nikolaizik WH, Trociewicz K, Ratjen F. Bronchial reactions to the inhalation of high-dose tobramycin in cystic fibrosis. Eur Respir J. 2002; 20:122-126.
Copyright: © 2025 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.