Journal of Medical Sciences and Health Care Research

Case Report - (2022) Volume 1, Issue 1
Presumed Toxoplasma Papillitis, Atypical Presentation, Diagnosis and Management: A Case Series in Indian Population
Received Date: Feb 03, 2022 / Accepted Date: Mar 10, 2022 / Published Date: Mar 17, 2022
Abstract
Ocular Toxoplasmosis (OT) is a form of infectious posterior uveitis with wide prevalence ranging from 2 to 23%. OT typically presents as a white grey retinitis lesion adjacent to an old scar with associated vitritis, vasculitis which involves both retinal veins and arteries. Unusual presentation in the form of optic nerve involvement has been described in literature with prevalence ranging from 5% to 12 %. We describe three such cases of presumed toxoplasma related papillitis, clinical features, investigations and their management outcomes. To the best of our knowledge, this is a unique cases series and first to be described in Indian population.
Keywords
Ocular toxoplasmosis, Toxoplasma papillitis, Visual fields, Azithromycin, Clindamycin
Abbreviations
OT: Ocular Toxoplasmosis; HVF: Humphrey Visual Fields; OCT: Optical Coherence Tomography
Introduction
Presumed toxoplasma papillitis is an unusual and atypical presentation where the predominant clinical features are blurring of vison, absence of dense vitritis, unilateral pallid disc edema with positive toxoplasma serology. We describe three such cases of papillitis with adjacent retinitis, their work up, clinical approach and management guidelines. An ethical committee clearance along with patient consent for using their data and images has been obtained
Case 1
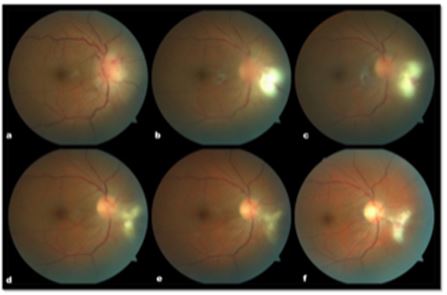
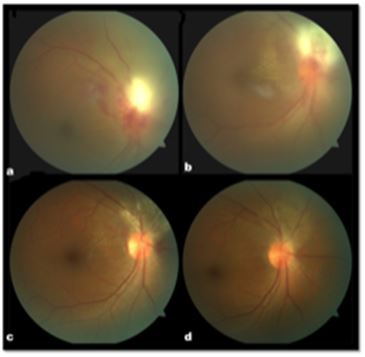
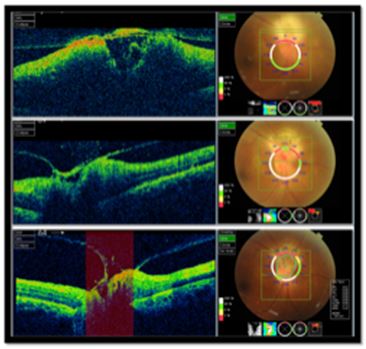
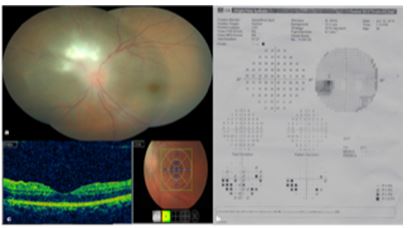
A 33-year-old male presented with complaints of floaters in right eye of 1 week duration associated with minimal blurring of vision. No associated redness, pain on ocular movements or headache. He had myopic refraction of -3.75 DS in both eyes with BCVA of 20/20, N6 in both eyes. Colour vision with ishihara chart was normal in both eyes. Systemic history was normal. Slit lamp examination in the right eye showed occasional cells in the anterior chamber, no flare, clear lens and cornea and a trace afferent pupillary defect. Left eye examination with fundoscopy was unremarkable. Intraocular pressure was 16 mm of Hg with Perkin’s tonometer. Fundus examination showed minimal vitritis, pallid disc edema with dilated blood vessels, vascular sheathing and superficial retinal hemorrhages in the nasal quadrant (Figure 1a) along with nasal shallow subretinal fluid. On Humphrey Visual Fields (HVF), right eye showed an enlarged blind spot, an absolute scotoma nasal to disc with break out to nasal periphery (Figure 2a ). Left eye was normal. Optical Coherence Tomography (OCT) showed edema of the optic disc with adjacent serous detachment. The diagnosis of inflammatory disc edema was made. He underwent blood investigations pertaining to uveitis along with neuroimaging plain and contract enhanced magnetic resonance imaging of brain, optic nerve and tracts. On the blood investigations panel, toxoplasma gondi IgG was found positive 4.67 (>1.1 positive) with IgM negative. Neuroimaging was normal.
FIG.1. Fundus examination in the nasal quadrant.
He was started on Tab Azithromycin 500 mg once a day along with Tab Clindamycin 300 mg twice a day for eight weeks as a presumed case of toxoplasma papillitis. Additionally, oral corticosteroids starting from 60 mg/day with weekly taper in 10 mg over a period of eight weeks in view of the serous detachment were given. Supportive treatment with oral antacids and lactobacillus was given. At end of 8 weeks course of disc edema resolved with cleared disc margins, scarred retinitis with resolved perivasculitis and serous detachment (Figure 1b-1e). On his follow up visit of 3 months patient visual acuity was 20/20 with resolved toxoplasma granuloma nasal to disc with persisting nasal scotoma (Figure 2).
Fig.2. Visual acuity.
Case 2
A 50 year old male with blurring of vision with a scotoma in right eye of 10 days duration. He was a known diabetic and hypertensive on treatment for 5 years. His Best corrected visual acuity was 20/30 and 20/20 in right and left eyes respectively. Anterior segment showed a trace afferent pupillary defect in the right eye with trace cells in the anterior chamber. Intraocular pressure with Perkins tonometry was 15 and 13 mm of Hg. Fundus examination showed palliddisc edema, dilated blood vessels with an area of retinitis 1-1.5 disc diameters in size, nasal to the optic disc with one margin in close approximation to optic disc with large serous detachment (7-8 disc diameters) in the nasal and superior quadrants adjacent to the lesion (Figure 3). Left eye showed Mild non proliferative diabetic retinopathy. HVF in the right eye showed an enlarged blind spot with inferonasal sectoral absolute scotoma with break out to periphery (Figure 2). OCT of the optic nerve and adjacent area showed an area ofserous detachment of retina with elevation of the disc (Figure 4a). His Toxoplasma gondii serology showed positivity for both Ig G and IgM. He was started on anti-toxoplasma regimen along with weekly tapering dosage of oral corticosteroids. By end of eight weeks the lesion scarred completely with resolution of vascular sheathing and serous detachment (Figure 3,4b-4c). His 3 months follow up showed complete scarring of the lesion with BCVA of 20/20 both eyes, however the repeat HVF showed a persisting scotoma (Figure 2).
Fig.3. Fundus examination adjacent to the lesion.
Fig.4. Anti-toxoplasma regimen.
Case 3
A 33-year-old female patient presented with blurring of vision and floaters in the left eye of 10 days duration. There was no history of progressive vision loss, redness, pain on ocular movements or headache. BCVA was 20/20 both eyes. Anterior segment evaluation was unremarkable with no anterior segment inflammation and left sided trace afferent defect. Colour vision on Ishihara was normal. She was seen at neuro-ophthalmology clinic and advised Magnetic Resonance Imaging of brain and orbits which was normal including orbital sections. Humphrey visual fields showed normal in right eye and left eye showed enlargement of blind spot with depressed field nasal quadrant with break out to nasal periphery corresponding to the retinitis lesion (Figure 5b). She was referred to retina clinic and fundoscopy showed pallid disc edema with an adjacent area of retinitis superonasal to optic disc (Figure 5a). There were 7-8 disc diameters of serous detachment in the peripapillary area nasal to the disc with adjacent vascular sheathing. Patient was evaluated as a case of inflammatory disc edema blood investigations were done, which showed toxoplasma IgG 3.06 (>1.1 positive) and IgM 2.66 (>1.1 positive). She was started on anti-toxoplasma regimen along with oral corticosteroids weekly taper for six weeks. She was reviewed at end of six weeks, where the lesion was completely scarred with visual acuity of 6/6, N6 in both eyes.
Fig.5. Pallid disc edema with an adjacent area of retinitis superonasal to optic disc.
Discussion
Papillitis as a presenting feature of toxoplasma can be a challenging diagnosis due to the various atypical clinical features. The most common presenting symptom is blurring of vision. There is presence of relative afferent pupillary defect in all three cases due to the involvement of anterior aspect of the optic nerve head and the significant edema involving the retinal nerve fibre layer. All the three patients were found to have field defect corresponding to the serous retinal detachment and an enlarged blind spot due to the papillitis [ 1-5]. Due to the RAPD and disc edema these cases are generally referred to a neuro-ophthalmologist for evaluation. However, there are signs on clinical examination which can help differentiate these into a probable infectious etiology.
Careful slit lamp examination showed, vitritis localised to the area of involvement, best seen on OCT in the form of hyper-reflective dots in vitreous, retinal vasculitis adjacent to the papillitis and in all three cases a shallow serous retinal detachment in the involved quadrants. Once the papillitis and optic nerve edema settles it unmasks the adjacent retinitis lesion making the diagnosis easier like in case 1. The vitritis in these cases is generally not as severe as in other cases of toxoplasma retinitis which also makes the diagnosis difficult. The OCT of the optic nerve head shows vitritis in the form of hyper-reflective dots (Figure 4a-c) above the thickened and edematous retinal nerve fiber layer giving a clue to its infectious etiology and warrant a detailed infectious work up. Ocular sarcoidosis and tuberculosis are generally to be ruled out in Indian population. Due to the endemic nature of toxoplasma in our population we included toxoplasma titre in the uveitis work up. All the three cases had seropositivity for toxoplasma in the form of IgG and IgM.
OCT of retina is a valuble tool in these patients both in diagnosis and follow-up. OCT of the adjacent quadrants revealed a serous detachment of the retina demonstrating the presence of inflammatory serous detachment which also correlated with the field defects in these patients. The treatment response as well as the dosage of corticosteroids can be titrated based on the resolution of subretinal fluid on the OCT as well as the clearing vitritis and nerve fiber layer edema of the optic nerve head. In the above three cases serial OCT (Figure 3) demonstrated the resolution of the subretinal fluid and the nerve fiber layer edema in response to anti toxoplasma regimen and oral corticosteroids.
Due to the presenting papillitis these three patients also had a detailed neurological work up rule out localised pathology involving the optic nerve which includes neuro imaging and relevant blood work up in their publication described toxoplasmic optic neuropathy characterized by subacute vision loss and optic nerve swelling accompanied by macular star [6]. Toxoplasmosis can produce multifocal lesions in the central nervous system with a predilection for the basal ganglia and the frontal, parietal, and occipital lobes. Intracranial calcification may be seen on Computed Tomography (CT). Magnetic resonance imaging (MRI) scanning typically shows multiple lesions that are isointense with the brain on TI-weighted images and isointense or hyperintense on T2-weighted images. In the above cases neuro imaging was unremarkable and has no intracranial lesions. The including of neurological imaging can be done on the basis of clinical assessment especially when the presentation is atypical and if visual acuity is not correlating with the clinical findings and also to rule out CNS lesions. In a large case series study by, optic nerve involvement was most commonly encountered as secondary to a distant active lesion, followed by cases secondary to the activation of an old peripapillary scar, and finally by cases resulting from direct involvement [3]. In contrast, reported active lesion sites in the juxta papillary region or in the region closest to the optic disc in all their patients with optic nerve involvement similar to our 3 cases [6,7].
The visual field examination in these cases shows an enlarged blind spot along with an absolute scotoma with break out to periphery suggested that retinochoroidal lesions within one-disc diameter of the optic disc is more commonly associated with an absolute visual field defect with breakout to the periphery than lesions further away which caused a relative scotoma [5]. Since the ganglion cells distant to the optic disc represent a wider area in the visual field, absolute scotoma development requires involvement of wider peripheral areas and not of central areas. The post-treatment persistence of these scotomas is thought to be due to remaining full-thickness atrophy despite the resolution of the active lesion. This was also seen in the follow up OCT where there was significant loss of inner retinal layers after the resolution of retinitis. The repeat visual fields in two of the three cases (Figure 4) showed persisting visual field defect in the nasal quadrant despite of complete resolution of the papillitis and adjacent retinitis supporting this theory. Absolute scotomas persist in the visual field after treatment in cases with optic nerve involvement even when the appearance of the optic disc is back to normal and no atrophy is observed clinically.
The anti-toxoplasma treatment in these cases is generally longer and requires a two drug regimen for successful treatment. The treatment regimen consists of oral azithromycin 500 mg given once a day, oral clindamycin 300 mg twice a day alone with oral lactobacillus supplementation twice a day to prevent pseudo membranous colitis along with oral corticosteroid therapy (1mg/ kg body weight) in weekly or two weekly tapering doses. The patients have to be reviewed two weekly to assess the response in terms of resolution of disc edema, vitritis, retinitis and also the resolution of sub retinal fluid both clinically as well as on optical coherent tomography. In our experience on an average these lesions took longer time to scar compared to retinitis lone and an average of 8 weeks of treatment is required.
Patients have to be educated on possible complications like diarrhoea especially with clindamycin. None of the above three developed such symptoms. The papillitis and adjacent retinitis generally scar within 6 to 8 weeks of treatment [8]. In their series indicated that average of 4-8 weeks of gradual resolution is seen similar to our series. The serous retinal detachment, vasculitis took longer time 8 weeks on average for complete resolution. The low dosage of corticosteroids (5 mg) was continued till complete resolution of the inflammatory signs. Scarring or cicatrisation of these lesions typically was seen to happen from the centre to the periphery.
In conclusion, this case series highlights the diagnosis of atypical toxoplasma papillits, the presence of absolute field defects which take long time to resolve, following up with OCT as a tool for resolution and a complete 6-8 week course of anti-toxoplasma drugs along with oral corticosteroids for managing the inflammatory serous detachment. However, the limitation of this study being the small number, and lack of repeat toxoplasma titres after the completion of treatment.
Declaration of Patient Consent
The authors certify that they have obtained the appropriate patient consent form. The patients understand that their names and initials will not be published with strict concealment of their identity.
Conflicts of Interest:
There are no conflicts of interest.
Financial Support and Sponsorship
Nil
References
- Singh R, Gupta V, Gupta A. Pattern of uveitis in a referral eye clinic in north India. Indian J Ophthalmol. 2004; 52:121.
- Rathinam SR, Namperumalsamy P. Global variation and pattern changes in epidemiology of uveitis. Indian J Ophthalmol. 2007; 55:173-183.
- Eckert G, Melamed J, Menegaz B. Optic nerve changes in ocular toxoplasmosis. Eye. 2007; 21:746-751.
- Mert S, Cakar OP, Mert KA. Optic nerve involvement in ocular toxoplasmosis: 12-year data from a tertiary referral center in Turkey. Arq Bras Oftalmol. 2019; 82(4):302-309.
- Stanford MR, Tomlin EA, Comyn O, et al. The visual field in toxoplasmic retinochoroiditis. Br J Ophthalmol. 2005; 89(7):812â?814.
- Alipanahi R, Sayyahmelli S. Acute papillitis in young female with toxoplasmosis. Middle East Afr J Ophthalmol. 2011; 18(3):249-251.
- Tugal-Tutkun I, Corum I, OtuÌ?k B, et al. Active ocular toxoplasmosis in Turkish patients: A report on 109 cases. Int Ophthalmol. 2005; 26(6):221-228.
- Folk, James C, et al. Presumed toxoplasmic papillitis. Ophthalmol. 1984; 91(1): 64-67.
Copyright: © 2025 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.